About Dr. Abhishek Kasha
Dr. Abhishek Kasha is a leading Interventional Cardiologist, widely recognized for his skill in complex angioplasties, advanced imaging-guided interventions, physiology-based PCI, and high-risk coronary procedures.
With a passion for precision-driven care, Dr. Kasha has brought world-class heart treatments to Rayalaseema, ensuring patients in the region do not need to travel far for advanced cardiology care. His work combines compassion with cutting-edge techniques, transforming outcomes for patients with challenging heart conditions.
📍 Consulting Location
ASTER Narayanadri Hospital
Tirupati, Andhra Pradesh
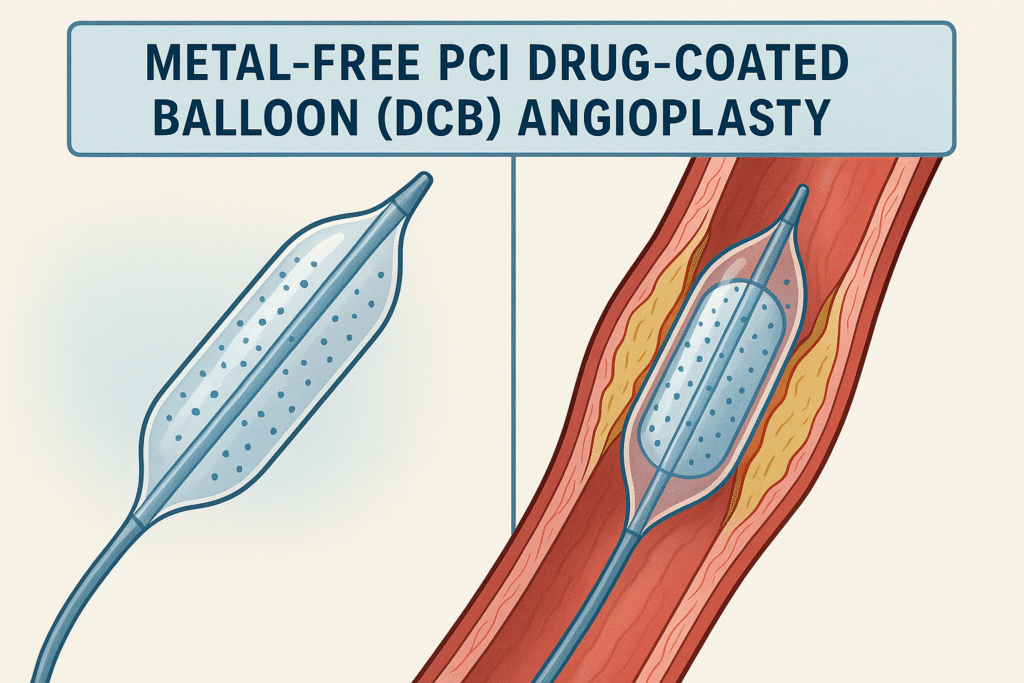
Metal-Free PCI with Drug-Coated Balloons (DCB): A New Frontier
What is “Metal-Free” PCI?
Traditional angioplasty often requires placing a metallic stent. While effective, stents can sometimes cause long-term issues such as late thrombosis, chronic inflammation, or complications if bypass surgery is needed later.
Drug-Coated Balloons (DCBs) represent a modern, “leave nothing behind” strategy. Instead of implanting a permanent scaffold, the balloon delivers an antiproliferative drug directly to the vessel wall during inflation—preventing restenosis without leaving metal behind.
Why this matters:
- Preserves natural vessel physiology.
- Reduces risk of late stent complications.
- Offers flexibility for future interventions.
- Allows for shorter duration of dual antiplatelet therapy (DAPT) in selected patients.
Strongest Evidence for DCB Use
- In-Stent Restenosis (ISR):
- Robust RCTs and meta-analyses show DCB is as effective as drug-eluting stents (DES) for ISR.
- Now guideline-endorsed globally.
- Small Vessel Disease (≤2.5–2.75 mm):
- Multiple randomized trials confirm DCB is safe and effective in small vessels where stenting is less ideal.
- Bifurcations & Ostial Lesions:
- Side-branch treatment with DCB is gaining traction.
- Calcified & Complex Lesions (with Atherectomy):
- Combining atherectomy or intravascular lithotripsy (IVL) with DCB shows promising results when guided by OCT/IVUS.
The Science Behind DCBs
- Mechanism: During balloon inflation (30–60 seconds), drugs like paclitaxel or newer sirolimus are delivered to vessel walls, preventing smooth muscle cell proliferation.
- Outcome: Maintains vessel openness, lowers risk of restenosis, and avoids permanent vessel caging.
Long-Term Outcomes
- Durability: Studies up to 3 years show low recurrence rates in ISR and small vessels.
- Safety: Eliminates very late stent thrombosis risk.
- Flexibility: Easier reintervention or CABG if needed.
However, patient selection and meticulous lesion preparation are critical. In complex lesions, a bail-out stent strategy must always be ready.
The Cath Team’s Approach: Checklist for Success with DCB
- Lesion Preparation: Aggressive pre-dilatation with NC/scoring balloons, atherectomy if calcified.
- Imaging Guidance: OCT/IVUS to assess calcium, dissection, and drug penetration.
- DCB Inflation: Proper sizing, 30–60 seconds inflation for maximum drug transfer.
- Bailout Readiness: DES implantation if severe recoil or flow-limiting dissection occurs.
- Tailored Antiplatelet Therapy: Shorter DAPT possible in elective cases with DCB-only strategy.
Future Directions
- Sirolimus-coated balloons: Showing promising safety and efficacy in early studies.
- Expanding Indications: Trials underway for large-vessel disease and ACS.
- Better Prep Tools: Intravascular lithotripsy + DCB could be the next big shift.
FAQs
1. What is the biggest advantage of metal-free PCI?
The biggest advantage is that no permanent metallic stent remains in your artery, which preserves natural vessel function and avoids complications like late thrombosis.
2. Is DCB available for all heart blockages?
Currently, DCB is best suited for in-stent restenosis, small vessels, and select complex lesions. For large arteries or acute heart attacks, stents are still the standard.
3. How safe is DCB compared to stents?
Clinical trials show that DCBs are as safe and effective as stents in specific conditions, with lower risks of late stent-related issues.
4. Do I need to take blood thinners for life after DCB?
Not always. In many elective cases, DCB-only therapy allows for shorter duration of dual antiplatelet therapy (sometimes just 1 month), especially if bleeding risk is high.
5. Will DCB make future surgeries easier?
Yes. Since there is no permanent implant, future bypass surgery (CABG) or re-interventions are technically simpler.