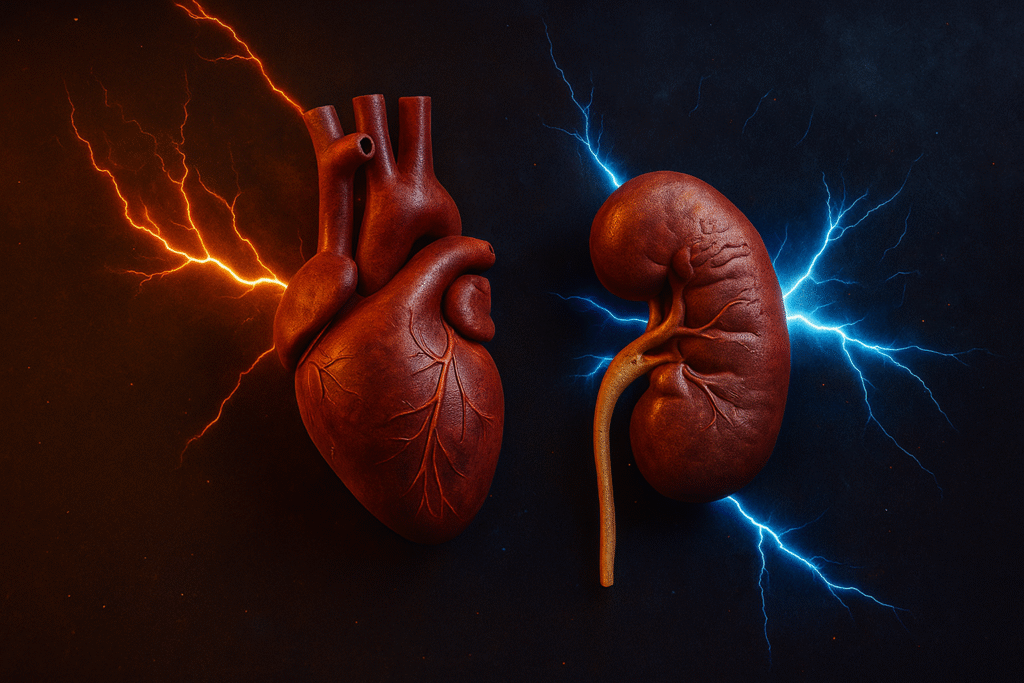
Chronic Kidney Disease (CKD) and Cardiovascular Disease (CVD) are two of the most significant global health challenges — and they are deeply connected.
People with kidney disease are far more likely to develop heart disease, while those with heart disease often experience kidney impairment over time.
This close interplay between the two organs has led experts to call them “the deadly duo.”
Understanding how these conditions interact can help prevent complications, improve outcomes, and save lives.
1. The CKD–Heart Disease Connection
CKD and CVD share multiple risk factors, including hypertension, diabetes, dyslipidemia, and systemic inflammation.
When the kidneys fail to filter waste effectively, toxins accumulate in the blood, causing vascular stiffness, volume overload, and increased cardiac strain.
Conversely, when the heart weakens, it fails to pump enough blood to the kidneys, leading to decreased filtration and progressive kidney damage — a mechanism known as cardiorenal syndrome.
The Bidirectional Relationship
- CKD to Heart Disease: Uremic toxins, anemia, and hypertension accelerate coronary atherosclerosis and heart failure.
- Heart Disease to CKD: Reduced cardiac output and congestion cause renal hypoperfusion and nephron injury.
2. How CKD Affects the Heart
CKD is an independent risk factor for cardiovascular events such as myocardial infarction, stroke, and sudden cardiac death.
Several mechanisms contribute to this increased risk:
- Atherosclerosis and Arterial Calcification: Caused by chronic inflammation and abnormal calcium-phosphate metabolism.
- Left Ventricular Hypertrophy (LVH): Due to long-standing hypertension and volume overload.
- Anemia: Low erythropoietin levels increase cardiac workload and lead to remodeling.
- Uremic Cardiomyopathy: Accumulation of uremic toxins impairs myocardial contractility and conduction.
3. How Heart Disease Damages the Kidneys
Cardiac dysfunction can directly cause or worsen kidney disease.
The main mechanisms include:
- Low Cardiac Output: Reduced renal perfusion impairs filtration.
- Venous Congestion: Increased renal venous pressure slows urine formation.
- RAAS Activation: Chronic stimulation leads to vasoconstriction and fibrosis.
- Medication Toxicity: Repeated exposure to contrast agents or aggressive diuretic use may worsen renal function.
This overlapping state is known as Cardiorenal Syndrome (CRS).
4. Cardiorenal Syndrome (CRS): The Overlap Zone
| Type | Primary Cause | Secondary Effect | Example |
|---|---|---|---|
| Type 1 | Acute cardiac failure | Acute kidney injury | Acute MI with renal shutdown |
| Type 2 | Chronic heart failure | Progressive CKD | Dilated cardiomyopathy with CKD |
| Type 3 | Acute kidney injury | Acute cardiac dysfunction | Sepsis-related AKI causing HF |
| Type 4 | Chronic kidney disease | Chronic heart failure | CKD causing LVH and HF |
| Type 5 | Systemic condition | Both heart and kidneys affected | Diabetes, sepsis, lupus |
5. Shared Risk Factors Between CKD and Heart Disease
- Hypertension: Both a cause and consequence of CKD and CVD.
- Diabetes Mellitus: The leading cause of CKD and a major driver of atherosclerosis.
- Dyslipidemia: Promotes vascular damage and accelerates plaque buildup.
- Smoking: Exponentially increases the risk of both diseases.
- Obesity and Metabolic Syndrome: Heighten cardiac and renal workload.
- Chronic Inflammation and Oxidative Stress: Contribute to endothelial dysfunction.
6. Recognizing the Clinical Clues
Symptoms of CKD with Cardiac Involvement
- Breathlessness and fatigue
- Swelling in legs or abdomen (edema)
- Chest discomfort or angina
- Palpitations from electrolyte imbalance
- Reduced or foamy urine output
Red Flags
- Rapid weight gain from fluid retention
- Resistant hypertension
- Rising creatinine after cardiac decompensation
Early recognition allows timely intervention before irreversible organ damage occurs.
7. Diagnostic Evaluation
Cardiac Workup
- ECG: To detect LVH, arrhythmias, or ischemia
- Echocardiogram: Evaluates ventricular function and valvular disease
- Coronary Angiography (if indicated): To assess for coronary artery blockages
Renal Workup
- Serum Creatinine and eGFR: To assess filtration function
- Urine Albumin-Creatinine Ratio (ACR): Detects early protein leakage
- Electrolytes: Monitor potassium, sodium, calcium, and phosphate
- Renal Ultrasound: For kidney size and structure
Biomarkers
NT-proBNP, cystatin C, and troponins can provide diagnostic clarity but must be interpreted cautiously in CKD patients.
8. Management Strategies: The Dual Approach
A. Optimize Cardiovascular Health
- Control blood pressure with ACE inhibitors, ARBs, or ARNI (monitored for kidney safety).
- Treat heart failure using diuretics, beta-blockers, MRAs, and SGLT2 inhibitors.
- Manage ischemia through revascularization or medication-based therapy.
B. Protect Kidney Function
- Maintain tight glycemic control (HbA1c <7%).
- Avoid nephrotoxins like NSAIDs and contrast agents.
- Follow a low-sodium, moderate-protein diet.
- Regularly monitor renal parameters and electrolytes.
C. Lifestyle and Prevention
- Restrict dietary sodium to under 2 grams per day.
- Engage in regular physical activity as tolerated.
- Avoid smoking and excess alcohol.
- Track daily weight and blood pressure.
9. Sexual and Psychosocial Health
Both CKD and CVD are associated with fatigue, reduced libido, anxiety, and depression.
- Address medication-related sexual dysfunction (e.g., beta-blockers).
- Encourage open communication and mental health support.
- Psychological counseling significantly enhances quality of life.
10. Nutrition and Lifestyle Recommendations
| Goal | Recommendation |
|---|---|
| Blood pressure control | Low-sodium, DASH-style diet |
| Kidney protection | Low phosphate, adequate hydration |
| Heart health | Limit saturated fats, increase omega-3 intake |
| Weight control | Regular activity and portion moderation |
| Avoid | Processed foods, high-salt snacks, NSAIDs |
11. Emerging Therapies and Research
Exciting developments in recent years have transformed cardiorenal management:
- SGLT2 inhibitors (empagliflozin, dapagliflozin) reduce hospitalizations and improve kidney outcomes.
- Finerenone, a non-steroidal MRA, slows CKD progression and reduces heart failure risk.
- Sacubitril/Valsartan (ARNI) improves both cardiac and renal outcomes.
- Novel biomarkers such as Galectin-3 and NGAL offer earlier detection of cardiorenal dysfunction.
12. When to Seek Urgent Medical Care
Immediate medical evaluation is required for:
- Sudden breathlessness or chest pain
- Rapid weight gain (>2 kg in 2–3 days)
- Swelling in legs or decreased urine output
- Palpitations or dizziness
Prompt care can prevent acute cardiorenal failure and hospitalization.
13. Preventing CKD and Heart Disease Together
Prevention remains the cornerstone of long-term protection:
- Regular screening of blood pressure, blood sugar, and lipids
- Annual kidney function tests for at-risk individuals
- Early initiation of medical therapy for diabetes and hypertension
- Patient education on diet, hydration, and medication adherence